Gm case 3
Patient was apparently asymptomatic 3 and half years back ,
then the patient had an episode of giddiness ,due to shock (from the death of his brother in law) ,for which he went to a local hospital and got diagnosed with hypertension.
Since then he was started on medication.He used to take the medication only when there's occasional neck stiffness and pain.
History of mild shortness of breath and chest pain 2 years back, which is not associated with cough or fatigue for which he went to a local hospital where he was told to have uncontrolled blood pressure.
Since then complaints were decreased in frequency but did not subsided.
Shortness of breath worsened 18 months back from exertion to even at less than ordinary activity Grade 2 to 3 which is associated with bilateral pedal edema, pitting type, upto the knees.
H/o fever 16 months back, associated with cough and weight loss cough relieved with medication.
In February 2022 patient presented to our hospital with complaints of worsened shortness of breath even at rest, Diagnosed to have Acute pulmonary edema secondary to heart failure and Renal Failure. Symptoms relieved and patient discharged with online follow up.
8 months back in view of refractory pulmonary edema and metabolic acidosis patient was initiated on hemodialysis and continuing maintainance hemodialysis regularly with frequency of 2-3 times per week.
Current admission:
Patient presented with Shortness of breath at rest and intermittent generalised body swelling and distension of abdomen since 6 months
Fever since 1 month
Shorteness of breath initially on exertion which gradually worsened even at rest associated with distension of abdomen.
Fever which is high grade, intermittent type associated with chills not associated with nausea, vomiting, altrered sensorium, cough and burning micturation.
PAST ILLNESS
No similar complaints in the past.
No significant medical or surgical history
Not a known case of DM, bronchial asthma, CAD, Epilepsy
FAMILY HISTORY:
No family history of HTN, DM, bronchial asthma, epilepsy
PERSONAL HISTORY :
Sleep disturbances since 6 months
Appetite improved since dialysis but decreased since distension of abdomen
Decreased urine output and no constipation.
Patient is a chronic alcoholic and chronic smoker since 15 years
Alcohol 90-150 ml per day whiskey/brandy
1-2 beedi per day for 15 years
Tobacco chewing daily Since 15 years
Examination :
Patient is conscious, coherent, cooperative.
Thin built and moderately nourished.
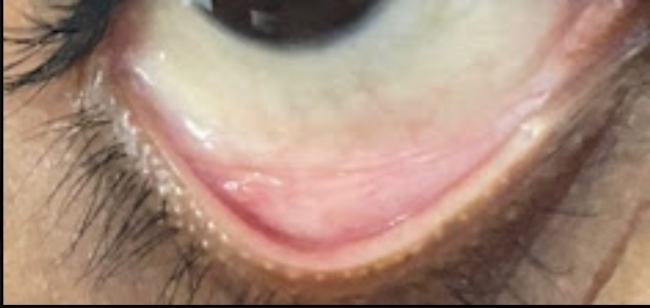
Pallor yes
Icterus no
Clubbing yes
Cyanosis yes
Lymphadenopathy no
Edema yes
Systemic examinations:
Respiratory system:
Inspection:
Upper respiratory tract -oral cavity,nose,oropharynx appears normal
Chest appears bilaterally symmetrical, elliptical in shape
Respiratory movements appear equal on both sides
Trachea Central in position and nipples are in 4th intercoastal space
No dilated veins ,scars,sinuses, visible pulsations
Palpation:
Trachea Central in position
Apical impulse in 5th intercoastal space 1cm medial to mid clavicular line
Chest circumference -31 inches at expiration 32 inches at full inspiration
Ap diameter 7 inches
Transverse diameter 12 inches
Percussion:
Supraclavicular-Resonant
Infraclavicular-Resonant
Mammary-Resonant
Infra axillary -Dull
Suprascapular-Resonant
Interscapular-Resonant
Infrascapular-Resonant
Auscultation:
Supraclavicular-Normal vesicular breath sounds
Infraclavicular: Normal vesicular breath sounds
Axillary -Normal vesicular breath sounds
Infraaxillary-wheezing breath sounds
Suprascapular-Normal vesicular breath sounds
Interscapular-Normal vesicular breath sounds
Infrascapular-wheezing breath sounds .
GIT EXAMINATION
Inspection:
Shape -Distended abdomen
Umbilicus-Everted
Equal symmetrical movements in all quadrants with respiration
No visible pulsations ,no scars
Palpation:
Local rise of temperature
Percussion:
Fluid thrills are present and shifting dullness
Auscultation:
Bowel sounds are not heard






Comments
Post a Comment