Gm case 4
CASE SCENARIO
HI,Im C.Srivally 3rd bds student .This is an online elog book to discuss our patients health data after taking his consent. This also reflects my patient centered online learning portfolio.
chief complaint
A 65 year old female daily labourer by occupation,resident of suryapet came to the opd with chief complaints of Fever and SOB since 3 days.
History of present illness
Pateint was apparently asymptomatic 3 days back then she developed fever high grade intermittent, associated with chills and rigors associated with body pains and weakness.
Patient was taken to near by hospital and was found to have high sugars and treated conservatively.
Patient also complaint about SOB since 3 days which is grade 2-3, increased on lying down and relieved by sitting.
No complaint of chest pain, palpitations
Normal urine output
No complaint of pedal edema, facial puffiness
Complaints of tingling sensation of hands and feet
Complaints of ulcer over Right foot after thorn pick injury
Five years ago patient developed giddiness for which she went to local hospital in suryapet and was diagnosis as Diabetic type 2.Since then she was on medication . 1 year ago she went for hospital for sudden left side paralysis which was diagnosed as CVA.
At the same time she was diagnosed with Hypertension and was on medication since then.
History of past illness
Patient is a known case of type 2 diabetes since 4 yrs.
On medication insulin from 1 year
Known case of hypertension 1 year and on medication
Known case of CVA Since 1 year with hemiperesis
And on medication
Not a known case of CAD, Thyroid disorders, Asthma and epilepsy.
Personal history
DIET: MIXED.
APPETITE: DECREASED
SLEEP: ADEQUATE.
BOWEL AND BLADDER: REGULAR
ADDICTIONS: NO ADDICTIONS
FAMILY HISTORY:
Not significant
SURGICAL HISTORY:
ABDOMINAL HISTERECTOMY 25 YEARS AGO
General examination::
Patient is conscious,coherent , cooperative
He is well built and moderately nourish
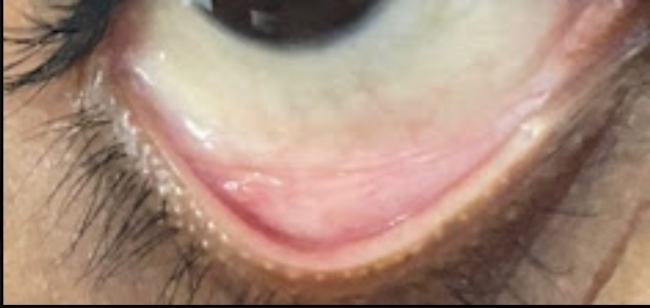
Pallor present
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: absent
Edema:absent
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM:
Inspection:-
Upper respiratory tract - oral cavity, nose & oropharynx appear normal.
Chest appears Bilaterally symmetrical & elliptical in shape
Respiratory movements appear equal on both sides and it's Abdominothoracic type.
Trachea central in position & Nipples are in 5th Intercoastal space
No dilated veins,sinuses, visible pulsations.
Palpation:-
All inspiratory findings confirmed
Trachea central in position
Apical impulse in left 5th ICS, 1cm medial to mid clavicular line
Percussion:
Supraclavicular -Resonant
Infraclavicular-Resonant
Mammary-Resonant
Infra axillary-Dull
Suprascapular-Resonant
Interscapular-Resonant
Infrascapular-Resonant
Auscultation:
Infraclavicular- (NVBS) (NVBS)
Mammary- (NVBS) (CREPTS)
Axillary- (NVBS) (NVBS)
Infra axillary-(NVBS) (CREPTS)
Suprascapular- (NVBS) (NVBS)
Interscapular- (NVBS) (NVBS)
Infrascapular- (NVBS)(NVBS)
GIT EXAMINATION
Shape of abdomen-scaphoid
Tenderness-No
Palpable mass-No
Liver- Not palpable
Spleen - Not palpable
Bowel sounds- Normal




Comments
Post a Comment